What are Fibroids?
Fibroids are non-cancerous growths that develop in or around the womb (uterus). The growths are made up of muscle and fibrous tissue, and vary in size. They're sometimes known as uterine myomas or leiomyomas. Many women are unaware they have fibroids because they don't have any symptoms.

Fibroids are a mixture of smooth muscle cells and fibroblasts, which form hard, round, whorled tumours in the myometrium. The pathophysiology of fibroids remains unknown, although it is hypothesised that each fibroid is derived from a mutation in a single smooth muscle cell.
The uterus is the commonest site for fibroids. The location may have an effect on symptoms and quality of life. For example, submucous fibroids may lead to heavy menstrual bleeding and fertility problems and large fibroids may occupy two or more locations and can extend from the endometrial cavity to the serosal surface.
How do I know I have Fibroids?
Women who do have symptoms (around 1 in 3) may experience:
- heavy periods
- Painful periods
- Tummy (abdominal) pain
- lower back pain
- Leg pains
- pelvic pain or mass
- a frequent need to urinate
- constipation
- pain or discomfort during sex
- In rare cases, further complications caused by fibroids can affect pregnancy or cause infertility.
Why fibroids develop
The exact cause of fibroids is unknown, but they have been linked to the hormone oestrogen. Oestrogen is the female reproductive hormone produced by the ovaries (the female reproductive organs). Increase in hormone oestrogen, and other sex steroid hormone, will influence the muscle and fibrous tissue to grow rapidly and spread from the myometrium. Fibroids usually develop during a woman's reproductive years (from around the age of 16 to 50) when oestrogen levels are at their highest. They tend to shrink when oestrogen levels are low, such as after the menopause when a woman's monthly periods stop.
What controls the growth of fibroids?
Oestrogen and progesterone control the proliferation and maintenance of uterine fibroids, and most medical treatments act by inhibiting the production of sex steroids or their action. The primary action of oestrogen is thought to be mediated through induction of progesterone receptor expression, thereby allowing leiomyomas to respond to progesterone. Hormonal replacement therapy may cause some growth of fibroids, but this is of uncertain clinical importance.
Who gets fibroids?
The prevalence of fibroids is estimated to be >70%. Risk Factors:
- Age: They most often occur in women aged 30 to 50
- Race and ethnicity: Fibroids are thought to develop more frequently in women of African-Caribbean origin
- Number of children (Parity): Women who have had children have a lower risk of developing fibroids, and the risk decreases further the more children you have
- Weight: It's also thought they occur more often in overweight or obese women because being overweight increases the level of oestrogen in the body.
- Dietary factors: Diet heavy in red mean is associated with a 70% increased risk of fibroids. Green vegetables, fruits, and dairy decrease the risk of fibroids.
- Family history: Genetics has a role in fibroid formation. If your mother or sister had fibroids, you are at an increased risk of developing them.
DIAGNOSING FIBROIDS
Fibroids are diagnosed through imagine (ultrasonography, X-ray, MRI), histological evaluation and biochemical laboratory evidence. Sometimes surgery is needed to confirm the diagnosis.
Fibroids are common, and with the widespread availability of high resolution ultrasonography, they are often diagnosed incidentally.
Women presenting in primary care with symptoms suggestive of fibroids should have their gynaecological history evaluated, including cervical screening, and should undergo a pelvic examination for any masses, a haemoglobin estimation to check for iron deficiency anaemia, and, if urinary symptoms are present, midstream urine testing to exclude a urinary tract infection. Diagnostic uncertainty, association with problematic symptoms, or any clinical or radiological suspicion of malignancy should prompt referral for further investigations. Women with asymptomatic fibroids, if the diagnosis is certain, often do not need further investigation or treatment.
 Left: An MRI axial or cross sectional scan. Right: An MRI sagital view of the pelvis. An MRI gives clinicians a reproducible, detailed picture of how many fibroids there are, how big they are and exactly where they are located. Not all women with fibroids need an MRI. All patients that are being evaluated for a uterine artery embolization will get an MRI.
Left: An MRI axial or cross sectional scan. Right: An MRI sagital view of the pelvis. An MRI gives clinicians a reproducible, detailed picture of how many fibroids there are, how big they are and exactly where they are located. Not all women with fibroids need an MRI. All patients that are being evaluated for a uterine artery embolization will get an MRI.
Types of fibroids
Fibroids can grow anywhere in the womb and vary in size considerably. Some can be the size of a pea, whereas others can be the size of a melon. The main types of fibroids are:
- Intramural fibroids are the most common type of fibroid, which develop in the muscle wall of the womb
- Subserosal fibroids develop outside the wall of the womb into the pelvis and can become very large
- Submucosal fibroids develop in the muscle layer beneath the womb's inner lining and grow into the cavity of the womb
In some cases, subserosal or submucosal fibroids are attached to the womb with a narrow stalk of tissue. These are known as pedunculated fibroids.
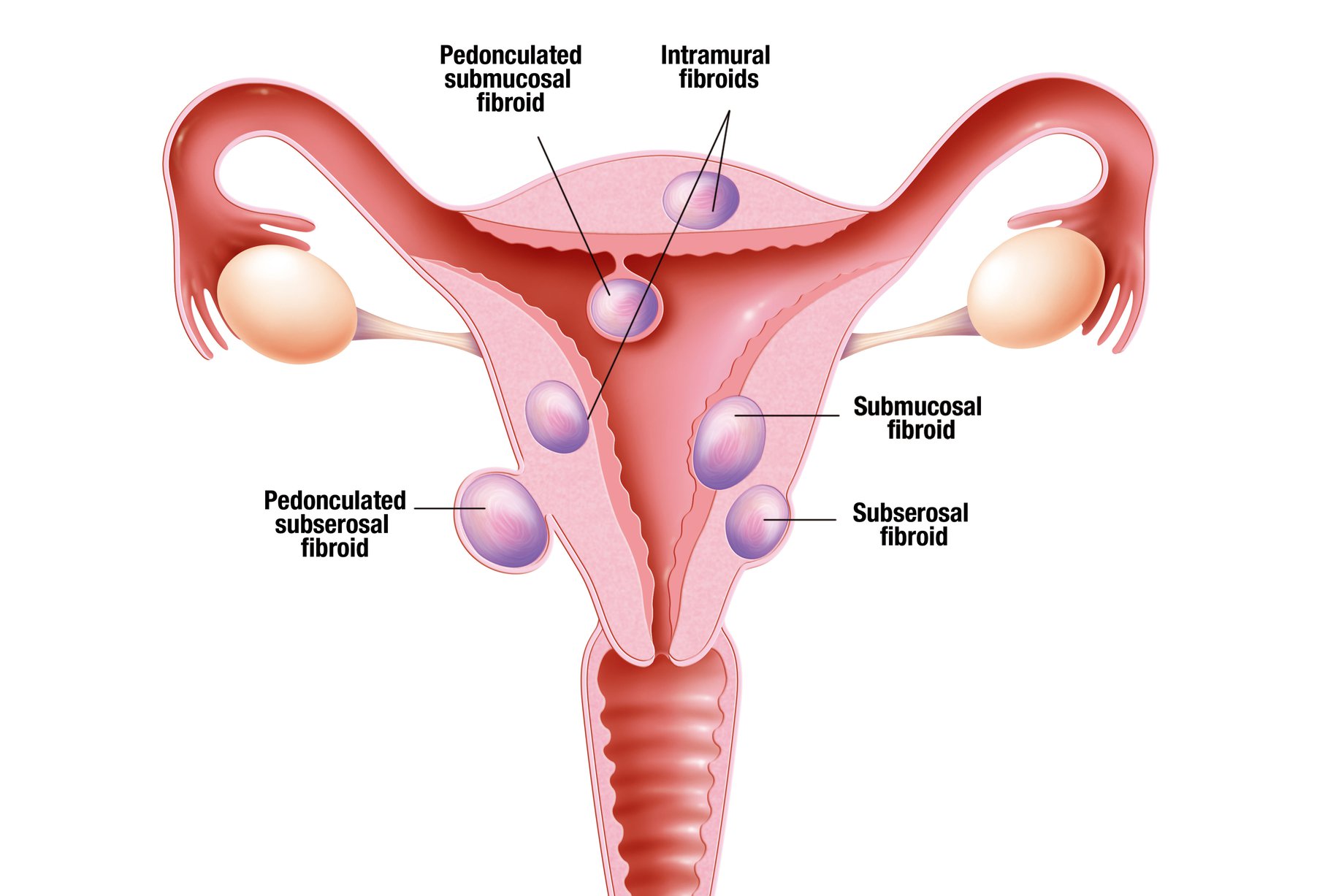 Diagram of the locations of uterine fibroids. Adapted from Mayo Foundation for medical education.
Diagram of the locations of uterine fibroids. Adapted from Mayo Foundation for medical education.
Treating fibroids
Fibroids don't need to be treated if they aren't causing symptoms. Over time, they'll often shrink and disappear without treatment, particularly after the menopause. If you do have symptoms caused by fibroids, medication to help relieve the symptoms will usually be recommended first. There are also medications available to help shrink fibroids. If these prove ineffective, surgery or other, less invasive procedures may be recommended.
Fibroids only require treatment when they cause symptoms. Hysterectomy, myomectomy, or uterine artery embolisation should be considered for fibroids (>3 cm) that cause heavy menstrual bleeding and affect quality of life. The most important clinical factor in determining any potential treatment option will be whether fertility or preservation of the uterus, or both, is desired. This usually steers the options between observational, medical, radiological, uterine preserving surgery, and hysterectomy.
Hysterectomy is the definitive method of resolving symptoms associated with uterine fibroids but is permanently contraceptive and is considered by many women to be more invasive than other methods.
Standard medical treatments for heavy menstrual bleeding may also be effective when such bleeding is associated with fibroids and may reduce the impact of heavy menstrual bleeding. There is less evidence supporting these medical treatments in the presence of uterine fibroids compared with heavy menstrual bleeding with normal uterine morphology.
| Treatment type | Advantages | Disadvantages |
| Medical treatment: | ||
| Tranexamic acid/mefenamic acid | Reduced heavy menstrual bleeding in women without uterine fibroids; improves health related quality of life | Efficacy in presence of fibroids is unknown |
| Levonorgestrol releasing intrauterine system | Treatment of choice for heavy menstrual bleeding in absence of fibroids; provides contraception | Evidence of usefulness in presence of fibroids is limited; cannot be used if uterine cavity is distorted by fibroids; high expulsion rate with submucosal fibroids |
| Selective progesterone receptor modulators | Reduces heavy menstrual bleeding and shrinks fibroids; does not cause menopausal side effect or bone demineralisation; licensed for preoperative use to shrink fibroids and for intermittent long term use | Can cause unscheduled bleeding in women with submucous fibroids; is associated with endometrial changes that are not yet fully understood |
| Mifepristone | Can reduce bleeding and pressure symptoms for up to six months; reduces heavy menstrual bleeding and improves fibroid related quality of life | Uncertain effect on fibroid volume |
| Gonadotrophin releasing hormone agonists | Can be used for 3-6 months presurgery to reduce uterine size, fibroid size, and perioperative blood loss; leads to amenorrhoea and helps correct iron deficiency anaemia; menopausal side effects can be minimised by the use of “add back” hormone replacement therapy | Long term therapy beyond six months can reduce bone density; vasomotor and other menopausal symptoms are common; more commonly initiated in secondary care, although continuation may take place in primary care |
| Radiological and surgical | ||
| Uterine artery embolisation | Performed under local anaesthesia (no general anaesthestic required); requires overnight stay in hospital; similar success rates and satisfaction rates to surgery; global uterine fibroid treatment; quick recovery; decreases fibroid size and menstrual blood loss; conserves uterus | Post-procedure pain can be severe and variable; alleviation of symptoms can take up to six months; risk of fibroid expulsion; higher rate of early re-intervention compared with surgery; impact on fertility and pregnancy is uncertain |
| Myomectomy | Conserves uterus; helps resolve bulk symptoms; can also be performed laparoscopically or | Insufficient evidence regarding role in improving infertility to conclude that it is best treatment; associated with major surgical risks; risk of fibroid regrowth; not a global uterine fibroid treatment; although morcellation of fibroids is possible at laparoscopic myomectomy, there are concerns about this treatment |
| Hysterectomy | Well established effective procedure to permanently resolve fibroid symptoms; cost effective with high patient satisfaction rates; vaginal and minimally invasive laparoscopic approach to this procedure is suitable in selected cases; global uterine fibroid treatment and only treatment that prevents recurrence; higher patient satisfaction rates than with uterine artery embolisation | Is associated with procedure related morbidity and mortality, whatever approach is used; higher surgical complication rates when associated with large fibroids; not suitable for women wanting to preserve fertility |
For more information on fibroids and the treatment of them, click here to see guidance from the British Medical Journal.
ARE THERE STUDIES I CAN BE INVOLVED IN?
Our research studies all focus around improving our understanding of endometriosis, working towards a non-surgical method of diagnosis and identifying new, better treatments. We have a number of research studies running that are recruiting patients. Read more...
FENOX
Aim – To identify the underlying mechanisms of endometriosis and uterine fibroids and their associated symptoms to improve the outcome of affected women.
In the FENOX study, we aim to improve our understanding of the underlying mechanisms of endometriosis and uterine fibroids and their associated symptoms by means of longitudinal observation and laboratory analyses. To achieve this, samples and clinical data are collected from women undergoing surgery. These samples are used in state-of-the-art biomedical research to improve our understanding of the underlying biology of these symptoms in women with endometriosis and/or fibroids, which will lead to a better understanding of the conditions, tailored therapies, and the development of biomarkers for diagnosis and treatment. Read more…

Patient Support
There are a number of endometriosis-related patient organisations that are available to offer information, guidance and support. Below is a selection of such organisations:
FibroidsConnect: A patient hub about uterine fibroids
The Lake Foundation: A UK charity that aims to improve the health of the African and African-Caribbean community through health promotion, early detection, research and support
British Fibroids Trust: A charitable organization that provides information on fibroids and treatment options, provides a platform for women to exchange their experiences
MORE INFORMATION
NHS information on diagnosing and treating fibroids
Guy's and St Thomas' NHS Trust 'Could you have fribroids' information leaflet
British Medical Journal clinical review on managing fibroids
National Institute for Health and Care Excellence (NICE) guidance on the management of fibroids
British Society of Interventional Radiology information on fibroids
Mayo Clinic information on the symptoms of fibroids and diagnosing and treating them

