The work, led by Dr Shishir Rao, Prof Kazem Rahimi and Mr Nouman Ahmed developed the model, called TRisk, which analyses a patient’s full medical history to estimate their likelihood of death within the next one to three years. By identifying patients at higher risk earlier, the system could help clinicians prioritise care, improve monitoring, and facilitate important discussions with patients and families. The findings have been published in npj Digital Medicine.
Addressing a major clinical challenge
Heart failure affects millions of people worldwide. It is a serious long-term condition where the heart does not pump blood as effectively as it should. While some people remain stable for years, others deteriorate more quickly.
Clinicians use risk scores to estimate a patient’s prognosis, but existing tools often rely on specialised tests such as heart imaging. These tests may not always be available and can be resource-intensive. Current models also struggle to account for the complex mix of other health conditions that many patients with heart failure have. Additionally, current models have focused on short- and long-term mortality prediction, unlike TRisk.
In fact, research shows that more than 40% of deaths in heart failure patients are linked to other medical problems rather than heart failure alone. The research team aimed to develop and test a system that could utilise routinely collected electronic health records (EHRs), including diagnoses, medications, and procedures, to deliver more accurate and practical mid-term risk predictions.
How TRisk works
TRisk uses a type of AI model known as a “Transformer” (i.e., the "T" in ChatGPT) which is designed to recognise patterns in sequences of data. Instead of focusing on a small number of measurements taken at a single point in time, TRisk analyses a patient’s entire medical journey.
By reviewing thousands of possible diagnoses, prescriptions and procedures recorded over many years, the model learns how combinations of conditions and events influence survival in heart failure patients. Importantly, TRisk does not require additional tests or new data collection, offering convenience to both patients and healthcare providers. It operates using information already recorded in routine healthcare systems.
Heart failure patients have complex health journeys that traditional risk models simply weren't designed to capture. TRisk changes that - it uses the medical information already sitting in routine care records to predict mortality and other clinical outcomes more accurately than existing tools, without requiring any additional tests or specialist referrals.
– Prof Kazem Rahimi, Professor of Cardiovascular Medicine and Population Health
TRisk's Validation
The model was developed using health records from over 400,000 patients with heart failure across England. It was then tested separately using US healthcare systems. When predicting death within 36 months (three years), TRisk was substantially more accurate than a widely used existing risk score (MAGGIC-EHR) adapted for electronic records.
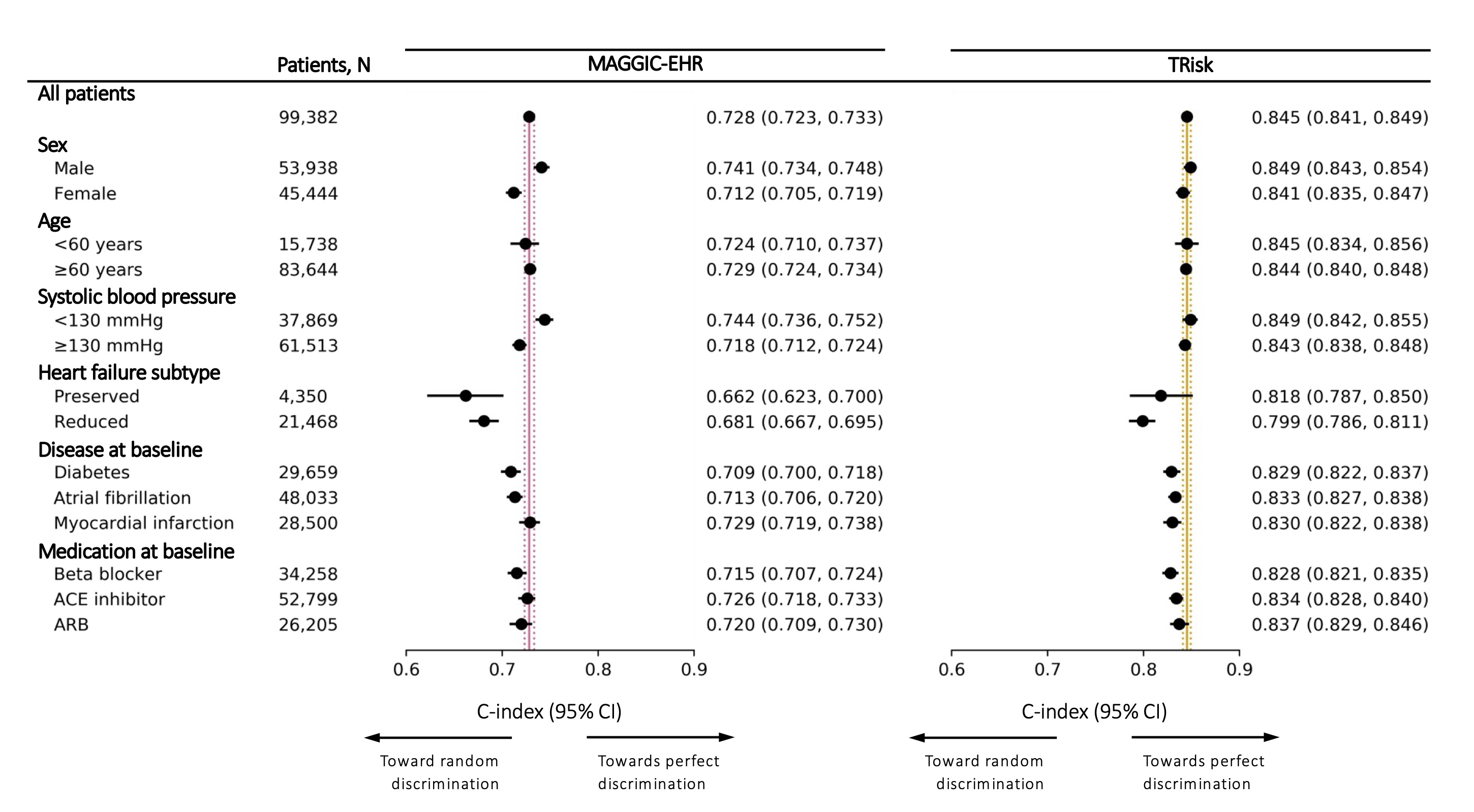
Figure 1. Models’ discrimination by concordance index (C-index) and associated 95% confidence intervals (CI) in overall cohort and subgroups for 36-month all-cause mortality risk prediction on UK validation data. Maroon and gold lines represent C-index on “all patients” in the validation cohort for MAGGIC-EHR and TRisk respectively. These solid and dotted coloured lines represent mean and 95% confidence interval boundaries of the overall cohort C-index for each model. These lines are provided to visually demonstrate deviation in subgroup discrimination performance from overall cohort performance for each model. ACE: Angiotensin-converting enzyme; ARB: Angiotensin receptor blocker.
The model also performed consistently across various age groups and sexes, indicating reduced bias in the modelling. When adapted for use in US hospital data, TRisk maintained strong predictive performance, demonstrating its potential scalability across different healthcare systems.
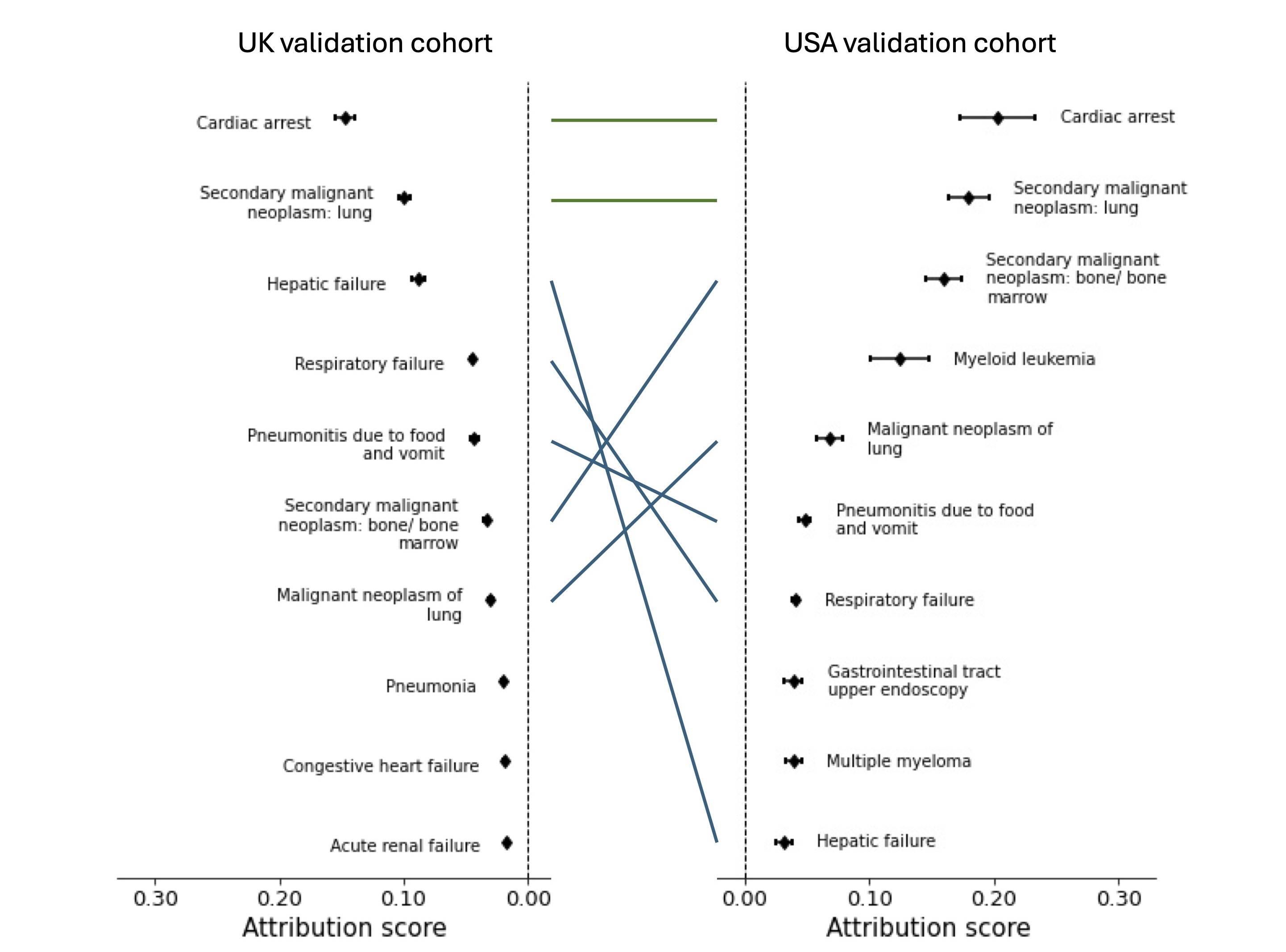
Figure 2. Average contribution for top ten encounters found as most contributing to mortality risk prediction on UK and USA validation cohort datasets. Point estimates of contribution values and associated 95% confidence intervals are presented for each encounter. We investigated encounters with top ten contribution scores as captured by our TRisk model across UK (left) and USA (right) datasets. Green line denotes both encounter and rank were preserved between validation analyses; blue line denotes only encounter was preserved.
What really excited us was that TRisk performed consistently across different patient groups - by sex, age, and clinical characteristics. In an era where we're rightly concerned about algorithmic bias in healthcare, this model shows we can build AI tools that work equitably.- Dr Shishir Rao, Senior Research Scientist; Deep Medicine AI Research Lead
New insights into risk factors
To better understand how the model was making decisions, the researchers conducted detailed analyses of which medical conditions most influenced risk predictions. The model identified well-known risk factors such as cardiac arrest.
However, it also highlighted the importance of conditions that are sometimes under-recognised in heart failure care, including cancers, liver failure and respiratory conditions. Interestingly, previous cancer diagnoses continued to influence mortality risk even when they had occurred more than ten years earlier. This finding may help inform future research into long-term health impacts in people living with multiple conditions.
The model confirmed something that has been hypothesised for some time: medical history of cancer or its treatment continues to influence mortality risk in heart failure patients even a decade later. That's the kind of insight that can only emerge when you let AI examine the full arc of a patient's medical history.
- Dr Shishir Rao, Senior Research Scientist; Deep Medicine AI Research Lead
Potential impact on heart failure care
The researchers suggest that TRisk is not designed to replace clinical judgement. Instead, it could serve as a decision-support tool.
TRisk has the potential to:
- Identify and support the appropriate monitoring of patients who may need additional support
- Support the prioritisation of treatments
- Support timely palliative care discussions where appropriate
- Manage lower-risk patients and prevent unnecessary interventions
Next steps
TRisk has been validated using historical data, but further work is needed before it can be introduced into routine clinical practice. This includes prospective studies to assess how using the model influences decision-making and patient outcomes, as well as local validation within specific healthcare settings.
Collaborators and Contributors
-
The work was conducted by colleagues from the Nuffield Department of Women’s & Reproductive Health, along with international collaborators. Shishir Rao, Kazem Rahimi, Nouman Ahmed, Mark Woodward, Nathalie Conrad, Christopher Yau, Gholamreza Salimi-Khorshidi, Huimin Su, Folkert W. Asselbergs, Rod Jackson, John G. F. Cleland.
- This research was supported by the HORIZON Europe AI4HF programme (Artificial Intelligence for Heart Failure). Further details are available here.
Publication
npj Digital Medicine (2026).